Журнал «Медицина неотложных состояний» Том 20, №7, 2024
Вернуться к номеру
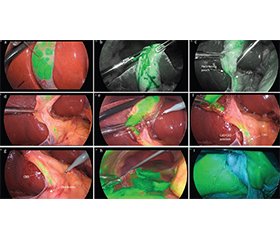
Як безпечно виконати лапароскопічну холецистектомію: анатомічні орієнтир
Авторы: Чуклін С.М., Чуклін С.С.
Медичний центр Святої Параскеви, м. Львів, Україна
Рубрики: Медицина неотложных состояний
Разделы: Клинические исследования
Версия для печати
Рівень ушкодження жовчних проток при лапароскопічній холецистектомії залишається вищим, ніж при відкритій холецистектомії. Інтраопераційні пошкодження здебільшого є результатом неправильної інтерпретації анатомічних структур через серйозне запалення або топографічні зміни. Стандартна лапароскопічна холецистектомія потребує правильної дисекції трикутника Calot для досягнення критичного погляду на безпеку (CVS — critical view of safety). CVS є кінцевим продуктом процесу дисекції, і пошкодження жовчних проток виникають до завершення цього процесу. CVS не завжди можна досягти у випадках тяжкого холециститу через технічні труднощі. Повна стратегія безпеки повинна включати раннє розпізнавання труднощів та ідентифікацію холецистектомій у випадках, коли неможливо досягти CVS, щоб використовувати нові інтраопераційні технології для уточнення анатомії. Фіксовані анатомічні орієнтири можуть допомогти в орієнтації для правильного визначення хірургічної анатомії під час операції. У цьому огляді міститься інформація про критичні орієнтири для оцінки розташування життєво важливих структур у скомпрометованих анатомічних умовах.
Bile duct injury rates in laparoscopic cholecystectomy remain higher than during open cholecystectomy. Intraoperative injuries are mostly the result of a misinterpretation of anatomical structures due to severe inflammation or topographical variations. Standard laparoscopic cholecystectomy requires proper dissection of Calot’s triangle to achieve the critical view of safety (CVS). The CVS is the end product of dissection, and bile duct injuries occur before the conclusion of that process. The CVS cannot always be achieved in cases of severe cholecystitis because of technical difficulties. A complete strategy of safety should therefore include early recognition of difficulties and identification of cholecystectomies, when the CVS cannot be achieved, in order to utilize new intraoperative technologies to clarify the anatomy. Fixed anatomical landmarks can help in proper orientation to ascertain the surgical anatomy correctly during surgery. Encompassed within the review are insights into identifying critical landmarks for assessing the positioning of vital structures in compromised anatomical conditions.
лапароскопічна холецистектомія; критичний погляд на безпеку; анатомічні орієнтири
laparoscopic cholecystectomy; critical view of safety; anatomical landmarks
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Pesce A, Palmucci S, La Greca G, Puleo S. Iatrogenic bile duct injury: impact and management challenges. Clin Exp Gastroenterol. 2019 Mar 6;12:121-128. doi: 10.2147/CEG.S169492.
- Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, et al. Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy. Ann Surg. 2020 Jul;272(1):3-23. doi: 10.1097/SLA.0000000000003791.
- de’Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021 Jun 10;16(1):30. doi: 10.1186/s13017-021-00369-w.
- Nassar AHM, Ng HJ, Wysocki AP, Khan KS, Gil IC. Achieving the critical view of safety in the difficult laparoscopic cholecystectomy: a prospective study of predictors of failure. Surg Endosc. 2021 Nov;35(11):6039-6047. doi: 10.1007/s00464-020-08093-3.
- Kaya B, Fersahoglu MM, Kilic F, Onur E, Memisoglu K. Importance of critical view of safety in laparoscopic cholecystectomy: a survey of 120 serial patients, with no incidence of complications. Ann Hepatobiliary Pancreat Surg. 2017 Feb;21(1):17-20. doi: 10.14701/ahbps.2017.21.1.17.
- Sgaramella LI, Gurrado A, Pasculli A, de Angelis N, Memeo R, Prete FP, et al. The critical view of safety during laparoscopic cholecystectomy: Strasberg Yes or No? An Italian Multicentre study. Surg Endosc. 2021 Jul;35(7):3698-3708. doi: 10.1007/s00464-020-07852-6.
- Deng SX, Greene B, Tsang ME, Jayaraman S. Thinking Your Way Through a Difficult Laparoscopic Cholecystectomy: Technique for High-Quality Subtotal Cholecystectomy. J Am Coll Surg. 2022 Dec 1;235(6):e8-e16. doi: 10.1097/XCS.0000000000000392.
- Nassar AHM, Nassar MK, Gil IC, Ng HJ, Yehia AM. One-session laparoscopic management of Mirizzi syndrome: feasible and safe in specialist units. Surg Endosc. 2021 Jul;35(7):3286-3295. doi: 10.1007/s00464-020-07765-4.
- Shang P, Liu B, Li X, Miao J, Lv R, Guo W. A practical new strategy to prevent bile duct injury during laparoscopic cholecystectomy. A single-center experience with 5539 cases. Acta Cir Bras. 2020;35(6):e202000607. doi: 10.1590/s0102-865020200060000007.
- Schendel J, Ball C, Dixon E, Sutherland F. Prevalence of anatomic landmarks for orientation during elective laparoscopic cholecystectomies. Surg Endosc. 2020 Aug;34(8):3508-3512. doi: 10.1007/s00464-019-07131-z.
- Iskandar M, Fingerhut A, Ferzli G. Posterior infundibular dissection: safety first in laparoscopic cholecystectomy. Surg Endosc. 2021 Jun;35(6):3175-3183. doi: 10.1007/s00464-020-08281-1.
- Sutherland F, Dixon E. The importance of cognitive map placement in bile duct injuries. Can J Surg. 2017 Dec;60(6):424-425. doi: 10.1503/cjs.008816.
- Smithmaitrie P, Khaonualsri M, Sae-Lim W, Wangkulangkul P, Jearanai S, Cheewatanakornkul S. Development of deep learning framework for anatomical landmark detection and guided dissection line during laparoscopic cholecystectomy. Heliyon. 2024 Jan 29;10(3):e25210. doi: 10.1016/j.heliyon.2024.e25210.
- Alius C, Serban D, Bratu DG, Tribus LC, Vancea G, Stoica PL, et al. When Critical View of Safety Fails: A Practical Perspective on Difficult Laparoscopic Cholecystectomy. Medicina (Kaunas). 2023 Aug 19;59(8):1491. doi: 10.3390/medicina59081491.
- Cheruiyot I, Nyaanga F, Kipkorir V, Munguti J, Ndung’u B, Henry B, et al. The prevalence of the Rouviere’s sulcus: A meta-analysis with implications for laparoscopic cholecystectomy. Clin Anat. 2021 May;34(4):556-564. doi: 10.1002/ca.23605.
- Abdelfattah MR. The Laparoscopic Anatomy of Rouviere’s Sulcus. Open Access Surgery. 2021;14:67-71. doi: 10.2147/OAS.S341710.
- Lockhart S, Singh-Ranger G. Rouviere’s sulcus-Aspects of incorporating this valuable sign for laparoscopic cholecystectomy. Asian J Surg. 2018 Jan;41(1):1-3. doi: 10.1016/j.asjsur.2016.07.012.
- Singh M, Prasad N. The anatomy of Rouviere’s sulcus as seen during laparoscopic cholecystectomy: A proposed classification. J Minim Access Surg. 2017 Apr-Jun;13(2):89-95. doi: 10.4103/0972-9941.201731.
- Ibrarullah M, Mohanty L, Mishra A, Panda A, Sikora SS. Anatomical appraisal of safe cholecystectomy: a prospective study. ANZ J Surg. 2023 May;93(5):1329-1334. doi: 10.1111/ans.18387. Epub 2023 Mar 15.
- Kumar A, Shah R, Pandit N, Sah SP, Gupta RK. Anatomy of Rouviere’s Sulcus and Its Association with Complication of Laparoscopic Cholecystectomy. Minim Invasive Surg. 2020 Aug 24;2020:3956070. doi: 10.1155/2020/3956070.
- Wang L, Hou H, Zhou D, He L. The hilar plane compared with the Rouviere’s sulcus plane during laparoscopic cholecystectomy. Wideochir Inne Tech Maloinwazyjne. 2022 Dec;17(4):660-671. doi: 10.5114/wiitm.2022.119236.
- Dahmane R, Morjane A, Starc A. Anatomy and surgical relevance of Rouviere’s sulcus. Scientific World Journal. 2013 Nov 6;2013:254287. doi: 10.1155/2013/254287. eCollection 2013.
- Jha AK, Dewan R, Bhaduria K. Importance of Rouviere’s sulcus in laparoscopic cholecystectomy. Ann Afr Med. 2020 Oct-Dec;19(4):274-277. doi: 10.4103/aam.aam_4_20.
- Du S, Qi Y, Zhao Y. Clinical application of Rouviere ditch to assist in the localization of cystic duct in laparoscopic cholecystectomy. J Laparosc Surg. 2017;22:939-941.
- Honda G, Hasegawa H, Umezawa A. Universal safe procedure of laparoscopic cholecystectomy standardized by exposing the inner layer of the subserosal layer (with video). J Hepatobiliary Pancreat Sci. 2016 Sep;23(9):E14-9. doi: 10.1002/jhbp.382.
- Gupta V, Jain G. Safe laparoscopic cholecystectomy: Adoption of universal culture of safety in cholecystectomy. World J Gastrointest Surg. 2019 Feb 27;11(2):62-84. doi: 10.4240/wjgs.v11.i2.62.
- Mischinger HJ, Wagner D, Kornprat P, Bacher H, Werkgartner G. The “critical view of safety (CVS)” cannot be applied — What to do? Strategies to avoid bile duct injuries. Eur Surg. 2021:53:99-105. doi: 10.1007/s10353-020-00660-1.
- Gupta V, Jain G. The R4U Planes for the Zonal Demarcation for Safe Laparoscopic Cholecystectomy. World J Surg. 2021 Apr;45(4):1096-1101. doi: 10.1007/s00268-020-05908-1.
- Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, et al. Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):73-86. doi: 10.1002/jhbp.517.
- Kitamura H, Fujioka S, Hata T, Misawa T, Yanaga K. Segment IV approach for difficult laparoscopic cholecystectomy. Ann Gastroenterol Surg. 2019 Nov 11;4(2):170-174. doi: 10.1002/ags3.12297.
- Fujioka S, Nakashima K, Kitamura H, Takano Y, Misawa T, Kumagai Y, et al. The segment IV approach: a useful method for achieving the critical view of safety during laparoscopic cholecystectomy in patients with anomalous bile duct. BMC Surg. 2020 Sep 23;20(1):214. doi: 10.1186/s12893-020-00873-x.
- Badawy A, Fathi I, Sabra T. D-line Approach for Safe Laparoscopic Cholecystectomy: Initial Experience. Cureus. 2023 Sep 10;15(9):e45003. doi: 10.7759/cureus.45003.
- Wang L, Zhou D, Hou H, Wu C, Geng X. Application of “three lines and one plane” as anatomic landmarks in laparoscopic surgery for bile duct stones. Medicine (Baltimore). 2018 Apr;97(16):e0155. doi: 10.1097/MD.0000000000010155.
- Wiboonkhwan NA, Thongkan T, Pitakteerabundit T. Photographic analysis of the anatomical landmarks in bile duct injury. ANZ J Surg. 2022 Jul;92(7-8):1955-1957. doi: 10.1111/ans.17426.
- Sebastian M, Sebastian A, Rudnicki J. The evaluation of B-SAFE and ultrasonographic landmarks in safe orientation during laparoscopic cholecystectomy. Wideochir Inne Tech Maloinwazyjne. 2020 Dec;15(4):546-552. doi: 10.5114/wiitm.2020.100972.
- Greene B, Tsang M, Jayaraman S. The inferior boundary of dissection as a novel landmark for safe laparoscopic cholecystectomy. HPB (Oxford). 2021 Jul;23(7):981-983. doi: 10.1016/j.hpb.2021.02.004.
- Tranter-Entwistle I, Eglinton T, Hugh TJ, Connor S. The artery first technique: re-examining the critical view of safety during laparoscopic cholecystectomy. Surg Endosc. 2023 Jun;37(6):4458-4465. doi: 10.1007/s00464-023-09912-z.
- Wijsmuller AR, Leegwater M, Tseng L, Smaal HJ, Kleinrensink GJ, Lange JF. Optimizing the critical view of safety in laparoscopic cholecystectomy by clipping and transecting the cystic artery before the cystic duct. Br J Surg. 2007 Apr;94(4):473-4. doi: 10.1002/bjs.5632.
- Mascagni P, Spota A, Felli E, Perretta S, Pessaux P, Dallemagne B, Mutter D. Conclusive Identification and Division of the Cystic Artery: A Forgotten Trick to Optimize Exposure of the Critical View of Safety in Laparoscopic Cholecystectomy. J Am Coll Surg. 2019 Nov;229(5):e5-e7. doi: 10.1016/j.jamcollsurg.2019.07.009.
- Samal D, Sahoo R, Mishra SP, Maiti KB, Patra K, Sahu MC. Cystic vein: a guide for safer laparoscopic cholecystectomy. Int Surg J. 2017;4:3238-41. doi: 10.18203/2349-2902.isj20174198.
- Hentati N, Fournier HD, Papon X, Aube C, Vialle R, Mercier P. Arterial supply of the duodenal bulb: an anatomoclinical study. Surg Radiol Anat. 1999;21(3):159-64. doi: 10.1007/BF01630893.
- Wang L, Hou H. The supraduodenal pedicle can be a useful landmark of the common bile duct in laparoscopic cholecystectomy. Wideochir Inne Tech Maloinwazyjne. 2021 Sep;16(3):620-621. doi: 10.5114/wiitm.2021.108213.
- Iftikhar M, Shah M, Ullah Z, Shakoor HA, Ullah S. Achie-ving Critical View of Safety via a New Technique: The Triple One (111) Technique. Cureus. 2023 Aug 25;15(8):e44098. doi: 10.7759/cureus.44098.
- Majumder A, Altieri MS, Brunt LM. How do I do it: laparoscopic cholecystectomy. Ann Laparosc Endosc Surg. 2020;5:15. doi: 10.21037/ales.2020.02.06.
- Alvarez FA, de Santibañes M, Palavecino M, Sánchez Cla–riá R, Mazza O, Arbues G, et al. Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. Br J Surg. 2014 May;101(6):677-84. doi: 10.1002/bjs.9486.
- Tomaoğlu K. Intraoperative Cholangiography in Laparoscopic Cholecystectomy: Technique and Changing Indications. İstanbul Med. J. 2020;21(5):350-354. doi: 10.4274/imj.galenos.2020.68366.
- Kovács N, Németh D, Földi M, Nagy B, Bunduc S, Hegyi P, et al. Selective intraoperative cholangiography should be considered over routine intraoperative cholangiography during cholecystectomy: a systematic review and meta-analysis. Surg Endosc. 2022 Oct;36(10):7126-7139. doi: 10.1007/s00464-022-09267-x.
- Goldstein SD, Lautz TB. Fluorescent Cholangiography Du–ring Laparoscopic Cholecystectomy: Shedding New Light on Biliary Anatomy. JAMA Surg. 2020 Oct 1;155(10):978-979. doi: 10.1001/jamasurg.2020.3003.
- Quaresima S, Balla A, Palmieri L, Seitaj A, Fingerhut A, Ursi P, Paganini AM. Routine near infra-red indocyanine green fluorescent cholangiography versus intraoperative cholangiography during laparoscopic cholecystectomy: a case-matched comparison. Surg Endosc. 2020 May;34(5):1959-1967. doi: 10.1007/s00464-019-06970-0.
- Dip F, LoMenzo E, Sarotto L, Phillips E, Todeschini H, Nahmod M, et al. Randomized Trial of Near-infrared Incisionless Fluorescent Cholangiography. Ann Surg. 2019 Dec;270(6):992-999. doi: 10.1097/SLA.0000000000003178.
- Dip F, Lo Menzo E, White KP, Rosenthal RJ. Does near-infrared fluorescent cholangiography with indocyanine green reduce bile duct injuries and conversions to open surgery during laparoscopic or robotic cholecystectomy? — A meta-analysis. Surgery. 2021 Apr;169(4):859-867. doi: 10.1016/j.surg.2020.12.008.
- Pesce A, Piccolo G, Lecchi F, Fabbri N, Diana M, Feo CV. Fluorescent cholangiography: An up-to-date overview twelve years after the first clinical application. World J Gastroenterol. 2021 Sep 28;27(36):5989-6003. doi: 10.3748/wjg.v27.i36.5989.
- Xie Q, Yang M, Jiang K, Zhang L, Mao T, Gao F. Laparoscopic cholecystectomy assisted by combined intravenous and intracholecystic fluorescent cholangiography: a case report. J Int Med Res. 2023 Dec;51(12):3000605231216396. doi: 10.1177/03000605231216396.
- Castagneto-Gissey L, Russo MF, Iodice A, Casella-Mariolo J, Serao A, Picchetto A, et al. Intracholecystic versus Intravenous Indocyanine Green (ICG) Injection for Biliary Anatomy Evaluation by Fluorescent Cholangiography during Laparoscopic Cholecystectomy: A Case-Control Study. J Clin Med. 2022 Jun 17;11(12):3508. doi: 10.3390/jcm11123508.
- Wang X, Teh CSC, Ishizawa T, Aoki T, Cavallucci D, Lee SY, et al. Consensus Guidelines for the Use of Fluorescence Imaging in Hepatobiliary Surgery. Ann Surg. 2021 Jul 1;274(1):97-106. doi: 10.1097/SLA.0000000000004718.
- Liu YY, Liao CH, Diana M, Wang SY, Kong SH, Yeh CN, et al. Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection: preliminary clinical results. Surg Endosc. 2018 Mar;32(3):1506-1514. doi: 10.1007/s00464-017-5838-9.
- Serban D, Badiu DC, Davitoiu D, Tanasescu C, Tudosie MS, Sabau AD, et al. Systematic review of the role of indocyanine green near-infrared fluorescence in safe laparoscopic cholecystectomy (Review). Exp Ther Med. 2022 Feb;23(2):187. doi: 10.3892/etm.2021.11110.
- Serban D, Smarandache AM, Cristian D, Tudor C, Duta L, Dascalu AM. Medical errors and patient safety culture — shifting the healthcare paradigm in Romanian hospitals. Rom J Leg Med. 2020;28(2):195-201. doi: 10.4323/rjlm.2020.195.
- Rabie OM. Evaluation of Methylene Blue in Difficult La-paroscopic Cholecystectomy. Int J Surg Res. 2019;8(1):5-10. doi: 10.5923/j.surgery.20190801.02.
- Gené Škrabec C, Pardo Aranda F, Espín F, Cremades M, Navinés J, Zárate A, Cugat E. Fluorescent cholangiography with direct injection of indocyanine green (ICG) into the gallbladder: a safety method to outline biliary anatomy. Langenbecks Arch Surg. 2020 Sep;405(6):827-832. doi: 10.1007/s00423-020-01967-z.
- Boogerd LSF, Handgraaf HJM, Huurman VAL, Lam HD, Mieog JSD, van der Made WJ, et al. The Best Approach for Laparoscopic Fluorescence Cholangiography: Overview of the Literature and Optimization of Dose and Dosing Time. Surg Innov. 2017 Aug;24(4):386-396. doi: 10.1177/1553350617702311.
- Tsutsui N, Yoshida M, Nakagawa H, Ito E, Iwase R, Suzuki N, et al. Optimal timing of preoperative indocyanine green administration for fluorescent cholangiography during laparoscopic cholecystectomy using the PINPOINT® Endoscopic Fluorescence Imaging System. Asian J Endosc Surg. 2018 Aug;11(3):199-205. doi: 10.1111/ases.12440.
- She WH, Cheung TT, Chan MY, Chu KW, Ma KW, Tsang SHY, et al. Routine use of ICG to enhance operative safety in emergency laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2022 Jun;36(6):4442-4451. doi: 10.1007/s00464-021-08795-2.
- Dili A, Bertrand C. Laparoscopic ultrasonography as an alternative to intraoperative cholangiography during laparoscopic cholecystectomy. World J Gastroenterol. 2017 Aug 7;23(29):5438-5450. doi: 10.3748/wjg.v23.i29.5438.
- Sebastian M, Rudnicki J. Recommendation for cholecystectomy protocol based on intraoperative ultrasound — a single-centre retrospective case-control study. Wideochir Inne Tech Maloinwazyjne. 2021 Mar;16(1):54-61. doi: 10.5114/wiitm.2020.93999.
- Conrad C, Wakabayashi G, Asbun HJ, Dallemagne B, Demartines N, Diana M, et al. IRCAD recommendation on safe laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci. 2017 Nov;24(11):603-615. doi: 10.1002/jhbp.491.