Резюме
Актуальність. За даними 2020 року, у світі налічується близько 400 мільйонів осіб із різними типами рідкісних захворювань, що включають понад 7000 нозологій. Дані офіційної статистики в багатьох країнах не дають докладної інформації про захворюваність на спадкові нервово-м’язові захворювання (СНМЗ); лише в країнах, що мають регістри пацієнтів із СНМЗ, можливо отримати детальну інформацію про захворюваність, смертність, аналіз генетичних причин, соціальні наслідки та ін. Матеріали та методи. Для оцінки ситуації з СНМЗ у Республіці Білорусь досліджували дитяче населення. Створено Республіканський центр спадкових нервово-м’язових захворювань (РЦ СНМЗ) для дітей, на базі якого сформовані комп’ютерна база даних і регістр СНМЗ. До популяції увійшли пацієнти віком від 0 до 18 років (включно 17 років 11 місяців 29 днів). Виконано ретроспективне суцільне порівняльне (за нозологіями) дослідження. Результати. На підставі даних регістру СНМЗ для дітей (0–17 років) встановлена поширеність СНМЗ у педіатричній популяції на 31.12.2020 року — 2,34 випадку на 10 000 населення відповідного віку. Результати показали, що при спінальній м’язовій атрофії (СМА) I типу медіана часу до встановлення діагнозу скоротилася майже втричі: так, якщо в період до 2019 р. Me = 7 місяців, то в 2019–2020 роках Me = 2,6 місяця, p ˂ 0,001. Також суттєво скоротилися терміни верифікації діагнозу СМА II типу: від Мe = 16 місяців (у період до 2019 р.) до Me = 7,5 місяця (2019–2020 рр.), p ˂ 0,05, що вказує на важливість створення централізованого РЦ СНМЗ для дітей у Республіці Білорусь і підтверджує необхідність роботи з розвитку його структури та взаємодії з іншими громадськими та державними організаціями. Висновки. У структурі нозологій СНМЗ лідирували міодистрофії Дюшенна — Беккера — 0,8 на 10 000 населення (0–17 років), СМА — 0,5 на 10 000 населення (0–17 років), спадкові полінейропатії — 0,4 на 10 000 населення (0–17 років). Частка народжених недоношеними (до 37 тижнів терміну гестації) із числа всіх дітей, зареєстрованих із СНМЗ, становила 6,4 %, при цьому найбільш висока відзначена у випадках СМА, що дає підставу розглядати недоношених новонароджених із позицій настороженості щодо СНМЗ. Висока питома вага в структурі СНМЗ, за даними регістру, в Республіці Білорусь належить дистрофінопатіям, які разом із попереково-кінцівковими міодистрофіями, фаціоскапулохумеральними м’язовими дистрофіями становили 40,8 % (178/436) від загальної кількості випадків СНМЗ у регістрі, досягаючи поширеності 0,95 на 10 000 населення (0–17 років).
Background. In many countries, problems of rare orphan diseases have recently been discussed, more specifically, hereditary neuromuscular diseases (HNMDs). As for 2020 data, there were about 400 million people worldwide suffering from different types of rare diseases which comprise over 7,000 nosologies. The data from official statistics in many countries do not provide detailed information on the prevalence of HNMDs; it is possible to obtain precise information on morbidity, mortality, analyses of genetic causes, social impact, etc. only in those countries that have registries of patients with HNMDs. Materials and methods. To evaluate the situation with HNMDs in the Republic of Belarus, the pediatric population was examined. The Republican Center for Hereditary Neuromuscular Diseases (RC HNMD) for children was founded, based on which there were formed a computer database and the registry of patients with hereditary neuromuscular diseases. The age of patients was 0 to 18 years old (including 17 years 11 months 29 days). The study was designed as a retrospective, entire, and comparative (by nosologies). Results. As of December 31, 2020, the HNMDs registry for children (0–17 years) demonstrated that the HNMDs prevalence was 2.34 cases per 10,000 age-matched population. The results showed that in type I spinal muscular atrophy the median time before diagnosis verification decreased almost 3-fold: before 2019 it was 7 months, while in 2019–2020, Me = 2.6 months; p < 0.001. Also, there is a significant reduction of the period for verification of the diagnosis of type II spinal muscular atrophy, i.e. from Me = 16 months (before 2019) to Me = 7.5 months (2019–2020), p < 0.05, which demonstrates the importance of establishing a centralized RC HNMD for children in Belarus and substantiates the necessity of developing its structure and cooperation with other community-based and government organizations. Conclusions. Within the structure of HNMDs nosologies, the top ones were taken by Duchenne-Becker muscular dystrophy — 0.8 per 10.000 age-matched population people spinal muscular atrophy — 0.5 per 10,000 of age-matched population, hereditary polyneuropathies — 0.4 by 10,000 of age-matched population. The study results show that the proportion of children born preterm (before 37 weeks of gestation) from the total amount of all children with registered HNMD accounts for 6.4 %, while the highest rate was found for spinal muscular atrophy, which gives the reason to study children born preterm from the standpoint of alertness due to HNMD. The register data in the Republic of Belarus demonstrate the highest specific weight of dystrophynopathies within the structure of HNMDs, which made 40.8 % (178/436) from the total number of HNMDs cases of Registry with the prevalence of 0.95 per 10,000 age-matched population (0–17 years) along with limb-girdle muscular dystrophies, facioscapulohumeral muscular dystrophies.
Introduction
Over the last few years, there has been a more active discussion of the issues of rare orphan diseases and, more specifically, hereditary neuromuscular diseases. Based on the available data, there are approximately 400 million people worldwide who suffer from various types of rare diseases whose number already includes over 7,000 disease entities [1].
Neuromuscular diseases are a diverse group of diseases among which a special place belongs to hereditary neuromuscular diseases (HNMDs). Each HNMD is rare, ho-wever, it has a medical, social, and economic significance for society. A significant social and economic burden dictates the necessity for the prediction of HNMD-related losses. The data from official statistics in many countries do not provide detailed information on the prevalence of HNMDs; it is possible to obtain detailed information on morbidity, mortality, analyses of genetic causes, social impact, etc. only in those countries that have registries of patients with HNMDs.
HNMDs present as muscle weakness, often cause significant changes in other organs and systems and lead to deterioration in daily functioning, disability and frequently to death during childhood. In addition, rare diseases with their onset during childhood create the necessity for constant caregiving, usually from a family member, which limits the healthy adult’s ability to work and, along with the necessity for constant caregiving, intensive and specialized care, causes significant indirect expenses for assistance and treatment of a patient suffering from an orphan disease. The situation regar-ding orphan diseases among children is aggravated by an unfavorable and progressive disease course with high mortality: specifically, it is estimated that approximately 30 % of children with rare diseases do not survive to the age of 5 [2]. The definition of an orphan disease varies depending on the country: in the US a disease is considered to be rare if its prevalence is 0.6 cases per 1,000 population [3]. The majority of countries define an orphan disease based on its prevalence: for example, in Europe, this is 50 cases per 100,000 population, which is equivalent to 1 : 2,000 in terms of prevalence [4]. The term “orphan (rare) diseases” has been introduced in the Republic of Belarus at a state level in 2020 as a part of the “Law on Medicinal Products” No. 13-Z dated May 13, 2020 [5]. According to this definition, orphan diseases are a group of severe chronic progressive disorders, generally of a genetic nature, having the level of population prevalence of not more than one case per 10,000 individuals and leading to a reduction in life expectancy and disability [5]. In addition, section 1 of this Law includes a definition of an orphan (rare) drug product, which is a drug product designed for diagnostics, etiopathogenetic or pathogenetic treatment (treatment aimed at the disease pathogenesis) of orphan (rare) diseases [5]. Therefore, from a legislative perspective, in the Republic of Belarus, a disease is considered to be orphan if its prevalence is not more than 1 per 10,000 individuals.
The data on the prevalence of HNMDs in children serve as an important basis for the determination of the extent of this problem, while the accurate and representative data on the prevalence and structure of these diseases are necessary for scientifically based healthcare planning by a diagnostic, treatment, and medical rehabilitation facility. Analyses of epidemiological studies and reliable data on the prevalence of HNMDs make it possible to ensure the scientific validity of the planning of treatment and prevention activities and the necessity for providing patients with medicinal products. One of the parameters that are important for statistical analysis is called “disease prevalence”, which is a medical and statistical parameter determining the prevalence of registered diseases (both newly emerged and previously existing) that were the reason for initial visits during a calendar year [6].
The prevalence of the same diseases in different countries may vary to a great extent and depend on a large number of factors, as well as reflect the specific features of a national gene pool. In recent years, considerable progress has been made in the diagnosis of HNMDs: according to the literature data, the most commonly occurring diseases among HNMDs are Duchenne muscular dystrophy with the prevalence of 1 per 3,500 to 1 per 5,000 newborn males, myotonic dystrophy with the prevalence of 0.5 to 18.1 per 100,000 [7, 8], and spinal muscular atrophy (SMA) that occurs approximately in 1 of 11,000 live births [9].
The purpose of our study is to investigate the pre-valence and structure of HNMDs in children (patients under 18 years old) in the Republic of Belarus for the year 2020.
Materials and methods
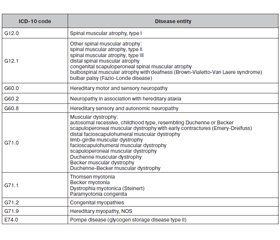
The pediatric population was studied to evaluate the situation concerning HNMDs in the Republic of Belarus. The study population included patients aged 0 to 18 years (including 17 years 11 months 29 days old). A retrospective comparative (by disease entities) study involving the entire population was carried out. The pediatric population with HNMDs was analyzed based on the data from the Republican Registry of HNMDs for patients under 18 years old. The Republican Center for Hereditary Neuromuscular Diseases for children served as a base for centralized registration of the data from all over the Republic of Belarus. The establishment of the Republican Center for Hereditary Neuromuscular Diseases for children and the initiation of its operation occurred in 2019 when a computer-based database of patients under 18 years old with HNMDs was developed for the first time; that database later served as a basis for the Registry of HNMDs for children and a register. The process of registration was carried out by disease entities that were coded under the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) based on which HNMDs are selected and grouped (Table 1).
/34.jpg)
Pompe disease (glycogen storage disease type II) does not belong directly to the HNMD group; however, considering that the clinical picture is dominated by a myopathic syndrome and that there is a pathogenetic enzyme replacement therapy available which, if administered in children propmtly, provides a favo-rable prognosis, this disorder is also included in the list of diseases that are the basis for referral of children to the Republican Center for HNMDs to determine the strategy for treatment and medical rehabilitation. In New Zealand, Pompe disease is also included in the country’s registry of HNMDs [10].
The study included patients under 18 years old, and every patient was a citizen/resident of the Republic of Belarus; an important inclusion criterion was the clinical diagnosis verification by genetic testing, as well as laboratory and neurophysiological tests. Cases with insufficient evidence (genetic testing in progress) were put into a separate group called “potential HNMDs”. The official data obtained from healthcare institutions of the Republic of Belarus served as a basis for creating a database for patients under 18 years old with HNMDs. Community-based organizations providing help for patients with HNMDs were also involved. In addition, a specially designed questionnaire was distributed in social media to facilitate the contact between the Republican Center for HNMDs and a patient with a possible HNMD and arrange a subsequent in-person consultation to verify or rule out a diagnosis. The data were collected for all territorial regions of the country: Mogilev, Grodno, Minsk, Brest, Gomel and Vitebsk regions and separately Minsk (city). First, demographic information and diagnosis data were collected for each new case; after confirming the diagnosis during an in-person consultation and obtaining an informed consent from parents or legal guardians of a patient under 18 years old, the data were entered in the Registry of HNMDs. Each child was assigned a unique number to avoid possible duplication of entries and to link each case to patient-specific information, clinical data, and diagnostic findings.
The prevalence by gender, age, region of residence, and diagnosis was calculated per 10,000 age-matched population (under 18 years old).
The obtained results were processed using a statistical software package Statistica v.6.1, as well as Microsoft Office Excel 2010. The results for qualitative characteristics are expressed in absolute figures, along with specifying the proportions (%).
Results
The analysis of the operation of the Registry of HNMDs for patients under 18 years old for the full calendar year allowed demonstrating its functionality because there is a well-conceived mechanism that regulates the flow of information on newly diagnosed cases of HNMDs and allows to actively evaluate the situation regarding the prevalence of a particular disease entity according to an age group of the population. As of December 2020, there were 436 patients under 18 years old with a HNMD clinical picture, and molecular genetic confirmation of the disease was available in all cases. The overall prevalence was 2.34 per 10,000 age-matched population (0 to 17 years old). The parameter was calculated using the following formula: K = A/B × × 10,000, where K is the parameter of interest (prevalence), A is the number of registered cases of HNMDs, and B is the average population aged 0 to 17 years. The data from the official statistical book on the annualized composition of the children population of the Republic of Belarus at the beginning of 2020 (without taking into account the population census) were used for calculations [11].
The researchers discuss a hypothesis that a genetic defect in the DNA of children with hereditary diseases may lead to a high rate of preterm births (before 37 weeks of gestation). In this regard, the birth histories related to the birth of children with HNMDs were analyzed sho-wing that 28 (6.4 %) of 436 children were born preterm (before 37 weeks) with a median gestation age of 34.5 weeks (Q25 = 31; Q75 = 35.5) in this group of preterm neonates. In the majority of cases (67.8 %; 19/28), the medical histories of these children included unpronounced muscular hypotonia from the first months of life. It should be pointed out that it is important to differentiate between muscle weakness and hypotonia when evaluating the muscular system. Hypotonia presents as a decrease in resistance with hypermobility of joints du-ring passive movements combined with a deteriorated ability to maintain antigravity postural motor control, while muscle weakness implies a decrease in muscle strength [12].
The analysis of the spectrum of HNMD entities showed a significant heterogeneity of the pathology in pediatric population; the data on the prevalence and structure of HNMDs are provided in Table 2.
/35.jpg)
A preliminary assessment of prevalence and its comparison with similar parameters from other European countries demonstrated the absence of any significant differences for many forms of HNMDs. Specifically, based on the international data, the prevalence of Du-chenne muscular dystrophy is 1 case per 5,000 male children [13], which is comparable to the figures seen in the Republic of Belarus, i.e. 1.5 cases per 10,000 male children. A comparison of the prevalence of SMA in the Republic of Belarus (0.5 per 10,000) with the figures from other countries (10 per 100,000 or 1 per 10,000 live births) [14] did not show any excess in the prevalence of this disease on the territory of the Republic of Belarus. At the same time, the prevalence of HNMDs in Northern Norway in the same age population (under 18 years old) is 57.8 per 100,000 (or 5.78 per 10,000) [15], which is 2 times higher than in the Republic of Belarus (2.34 per 10,000), while the figures for SMA are practically similar, with a slight excess in the Republic of Belarus compared to Northern Norway [15]: 0.5 per 10,000 and 0.37 per 10,000 (or 3.7 per 100,000), respectively. In the Republic of Belarus, a low prevalence of hereditary neuropathy in the pediatric population (0 to 17 years old) is noted, i.e. 0.4 per 10,000, while in Northern Norway [15] it is 29.9 per 100,000 (2.9 per 10,000) patients in the same age group. It should be noted that the parameter of the prevalence of hereditary neuropathies also included the forms of hereditary neuropathy with susceptibility to pressure palsies, including familial cases [16]. There are also registered cases of congenital myopathies that are heterogeneous in terms of a genetic defect and some instances require a longer period to confirm the diagnosis despite the occurrence of clinical manifestations from the moment of the child’s birth [17], which may be due to population features, as well as the issues of interpretation of diagnostic findings, choice of examination techniques, etc.
It should be taken into account that when collecting information for the Registry, some children may not be recorded in the healthcare institutions’ databases with the diagnosis of a hereditary disease due to parents’ unwillingness to submit the results of genetic testing according to the child’s place of registration, disagreement with and psychological unwillingness to accept the HNMD diagnosis, and other reasons. Specifically, the data from the Registry of hereditary neuromuscular diseases of the Republic of Belarus revealed 19 of such cases out of 436 (4.4 %), which requires optimization to ensure proper transitions of care, recruiting psychology specialists to the team, as well as informing medical specialists about new methods for diagnosis and treatment of rare diseases.
In addition, an analysis was carried out based on the time of HNMD diagnosis, which is a period from the moment of occurrence of first clinical manifestations of HNMDs in a child to the moment of the diagnosis confirmation; the assessment included patients with previously confirmed diagnoses (before 2019) and patients with the primary diagnosis of HNMD in 2019–2020. This division was due to the start of the operation of the Republican Center for HNMDs, training of subject-matter experts and actively informing medical specialists from various healthcare organizations about HNMDs in children, the existence of new treatment methods and the necessity for fast diagnosis so that therapy can be started as early as possible. The results showed that the median time to diagnosis confirmation for type I spinal muscular atrophy decreased almost three-fold: before 2019 it was 7 months, while in 2019–2020 Me = 2.6 months; p ˂ 0.001. In addition, there is a significant reduction of the period for verification of the diagnosis of type II spinal muscular atrophy, i.e. from Me = 16 months (before 2019) to Me = 7.5 months (2019–2020), p ˂ 0.05, which demonstrates the importance of establishing the centralized Republican Center for HNMDs for children in the Republic of Belarus and supports the necessity for working on developing its structure and cooperation with other community-based and government organizations.
Conclusions
1. Based on the data from the Registry of HNMDs of the Republic of Belarus for children (0 to 17 years old), the prevalence of HNMDs in the pediatric population as of December 31, 2020, was 2.34 cases per 10,000 age-matched population.
2. Within the structure of HNMD entities, the top ones were Duchenne-Becker muscular dystrophy with 0.8 per 10,000 population (0 to 17 years old), spinal muscular atrophy with 0.5 per 10,000 population (0 to 17 years old), and hereditary polyneuropathies with 0.4 per 10,000 population (0 to 17 years old).
3. According to the study results, the proportion of preterm born children (before 37 weeks of gestation) among all registered children with HNMDs was 6.4 %, while the highest proportion was observed for spinal muscular atrophy.
4. According to the data from the Registry, the highest percentage within the structure of HNMDs in the Republic of Belarus belongs to dystrophinopathies that, along with limb-girdle muscular dystrophies and facioscapulohumeral muscular dystrophies, accounted for 40.8 % (178/436) of the total number of HNMD cases, with the prevalence of 0.95 per 10,000 population aged 0 to 17 years old.
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Received 04.05.2021
Revised 13.05.2021
Accepted 22.05.2021
Список литературы
1. RARE Facts. Global genes. Available from: https://globalgenes.org/rare-facts/. Accessed July 20, 2020.
2. Angelis A., Tordrup D., Kanavos P. Socio-economic burden of rare diseases: a systematic review of cost of illness evidence. Health Policy. 2015. 119 (7). 964-979.
3. Babac A., Damm K., Graf von der Schulenburg J.M. Patient-reported data informing early benefit assessment of rare di-seases in Germany: A systematic review. Health Econ. Rev. 2019. 9 (1). 34.
4. Badia X., Gil A., Poveda-Andrés J.L., Shepherd J., Tort M. Analysing criteria for price and reimbursement of orphan drugs in Spain. Farm. Hosp. 2019. 43 (4). 121-127.
5. National Legal Internet Portal of the Republic of Belarus. 19.05.2020. 2/2732.
6. Prevalence definition. https://www.medicinenet.com/prevalence/definition.htm
7. Campbell C., Levin S., Siu V.M., Venance S., Jacob P. Congenital myotonic dystrophy: Canadian population-based surveillance study. J. Pediatr. 2013. 163 (1). 120-5, e1-3.
8. Theadom A., Rodrigues M., Roxburgh R. et al. Prevalence of muscular dystrophies: A systematic literature review. Neuroepidemio-logy. 2014. 43 (3–4). 259-68.
9. D’Amico A., Mercuri E., Tiziano F.D., Bertini E. Spinal muscular atrophy. Orphanet J. Rare Dis. 2011. 6. 71.
10. Rodrigues M.J., O’Grady G.L., Hammond-Tooke G. et al. The New Zealand Neuromuscular Disease Patient Registry; Five Years and a Thousand Patients. J. Neuromuscul. Dis. 2017. 4 (3). 183-188.
11. Healthcare in the Republic of Belarus [Electronic edition]: official. stat. coll. for 2019 Minsk: GU RNPC MT, 2019. 257 p.
12. Evtushenko S.K., Morozova S.K., Shaimurzin M.R. Muscular hypotension syndrome in newborns and young children. News of Medicine and Pharmacy. 2011. 384. 50-63.
13. Cowen L., Mancini M., Martin A., Lucas A., Donovan J.M. Variability and trends in corticosteroid use by male United States participants with Duchenne muscular dystrophy in the Duchenne Registry. BMC Neurol. 2019. 19 (1). 84.
14. Verhaart I.E.C., Robertson A., Wilson I.J. et al. Prevalence, incidence and carrier frequency of 5q-linked spinal muscular atrophy — a literature review. Orphanet J. Rare Dis. 2017. 12 (1). 124.
15. Müller K.I., Ghelue M.V., Lund I., Jonsrud C., Arntzen K.A. The prevalence of hereditary neuromuscular disorders in Northern Norway. Brain Behav. 2021. 11 (1). e01948.
16. Osadchuk T.V., Rumyantseva N.V., Naumchik I.V., Likha-chev S.A., Pleshko I.V., Shalkevich L.V., Zhаuniaronak I.V., Kachan Yu.P. Molecular genetic diagnosis and clinical characteristic of hereditary neuropathy with predisposition to palsy due to compression. 2016. 116. 1. 64-69.
17. Zhаuniaronak I.V., Shalkevich L.V., Kuznetsova A.V. Clinical and genetic heterogeneity of congenital myopathies. Medical News. 2020. 1 (304). 20-22.
/34.jpg)
/35.jpg)