Международный неврологический журнал 4 (74) 2015
Вернуться к номеру
Perinatal risk factors hypoxic-ischemic encephalopathy in term infants with normal and low to the gestational age body weight
Авторы: Ye.P. Ortemenka - The Department of Pediatrics and pediatric infectious diseases, Bukovinian State Medical Universi-ty, Chernivtsi, Ukraine
Рубрики: Неврология
Разделы: Клинические исследования
Версия для печати
Currently hypoxic-ischemic encephalopathy (HIE) of newborns takes a leading position (47% of cases) among all perinatal central nervous affections. However, data on the features of intrauterine and extrauterine fetal development periods of the term low birth weight (LBW) newborns with HIE are still limited and a predicting role of the perinatal factors in the realization of such comorbid condition has not been studied enough.
The aim. To study the role of intrauterine and extrauterine risk factors in the development of hypoxic-ischemic encephalopathy in term infants with normal and low to gestational age birth weight.
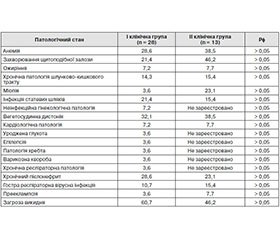
Materials and methods. In the department of neonatal pathology of the Chernovtsy Regional Children Clinical Hospital 41 newborns with hypoxic-ischemic encephalopathy have been examined. The first (I-st) clinical group has been formed from 28 term neonates with corresponding to gestational age body weight. The second (II-nd) clinical group included the remaining 13 low birth weight newborns. The comparison groups did not differ significantly on the main (sex and age) clinical characteristics. All neonates have been admitted in acute period of HIE and leading neurological syndrome of central nervous system depression (92,9% of patients in I-st clinical group and 92,3% of newborns in the II-nd comparison group).
These survey results have been analyzed by parametric (Pt, Students’ criteria) and nonparametric (Pφ, Fisher's angular transformation) methods of biological statistics.
Results. In low birth weight neonates the concomitant pathological conditions have been recorded significantly more often. Thus, comorbid conditions were diagnosed in 2 patients (7,2%) in the I-st clinical group, but only in 8 cases (61,5%) in the II-nd comparison group (P <0,01). And, at the same time, almost half (46,2%) of LBW newborns have had mothers living in urban areas, but in the I-st group only 17,9% of mothers were urban inhabitants (Pφ <0,05).
Analysis of the data indicates that the pregnancy of mothers of newborns with intrauterine retardation proceeded more often on the background of anemia (38,5%), thyroid pathology (46,2%), myopia (23,1%) and preeclampsia (7,7%) as compared to the II-nd group, in which these maternal pathological conditions occurred with a frequency of 28,6% (Pφ> 0,05), 21,4% (Pφ> 0,05), 3,6% (Pφ> 0,05) and 3,6% (Pφ> 0,05) respectively.
Newborn infants from I-st group of supervision were born as a result of pathological delivery (by cesarean section, vacuum-assisted delivery or by the help of drug induction) are twice as likely (32,1% of cases) to the II-nd comparison group (15,4% of cases Pφ> 0,05).
An thus, tight nuchal cord with development of the newborns’ distress during delivery has been occurred in a quarter (25%) infants of I-st clinical group, but only in one (7,7%) LBW neonates (Pφ <0,05). At the same time, pathological amniotic fluids (thick, meconial or hemorrhagic) have been registered in a third (32,1%) cases of the I-st clinical group versus 7,7% of cases in the comparison group (Pφ <0,05).
Severe asphyxia (Apgar 1-st minute score ≤ 4 points) has been diagnosed in every fifth (22,2%) patients of the I-st clinical group and only in 7,7% cases among LBW newborns (Pφ> 0,05). At once, in neonates with low to gestational age body weight after the first minute of life the respiratory problems, requiring artificial lung ventilation, have been occurred twice as often (61,5% of newborns in the II-nd group vs. 35,7% of infants in the I-st clinical group, Pφ <0,05).
In the early neonatal period some newborns (14,3% of cases in the I-st group and 7,7% of children in the II-nd group; Pφ> 0,05) postasphyctic multiple organ dysfunction syndrome has been developed, while only representatives of the I-st clinical group have had convulsive syndrome (17,9% of infants) compared with no cases in the II-nd group of supervision. At one time, according to the ultrasound of the heart, in the first ten days of life the signs of overload of the right heart chambers have been registered in every third newborns of the I-st clinical group (28,6%), but only in 7,7% of cases in the II-nd comparison group (Pφ <0,05) .
In the early neonatal period the concomitant problems of infant feeding (poor sucking, reduced food tolerance, regurgitation) were recorded twice more often in LBW newborns (61,5% of cases) in comparison with the I-st group (32,1% of infants; Pφ <0,05).
Conclusions. The main predictors of hypoxic-ischemic encephalopathy in term low birth weight neonates are: mothers’ residence in urban areas (46,2%); presence of chronic maternal disease (anemia, thyroid disease) during pregnancy (46,6%); concomitant congenital malformations in the one-third (30,8%) of infants; development of respiratory disorders at birth, requiring artificial lung ventilation (61,5%); infants’ feeding problems (61,5%).
The main risk factors preceding hypoxic-ischemic central nervous system injury in term neonates with adequate to gestational age body weight are: pathological course of intrapartum period (development of fetal distress due to tight nuchal cord in a a quarter of infants, as well as pathological delivery in a third (32,1%) cases of supervision, associated in the every third of newborns with acute asphyxia (Apgar 1-st minute test constellation ≤ 4 points), which often led to the development of cardiogenic complications (28,6%), multiple organ failure syndrome (14,3%) and seizures (17,9%).
1. Pal'chyk A.B. Hypoksychesky-yshemycheskaya entsefalopatyya novorozhdennih / A.B. Pal'chyk, N.P. Shabalov. – 4-e yzd., yspr. y dop. – M.: MED-press-ynform, 2013. – 288 s.
2. Posledstvyya perynatal'nikh porazhenyy tsentral'noy nervnoy systemi: dyskussyonnie voprosi / A.P. Volosovets, S.P. Kryvopustov, Y.A. Lohynova, M.A. Shakot'ko // Zdorov'e rebenka. – 2008. - #4 (13). – S. 101-106.
3. Antepartum and Intrapartum Factors Preceding Neonatal Hypoxic-Ischemic Encephalopathy M. Martinez-Biarge, J. Diez-Sebastian, C.J. Wusthoff, E. Mercuri, F.M. Cowan Pediatrics 2013;132;e952; originally published online September 9, 2013; DOI: 10.1542/peds.2013-0511
4. Risk factors for hypoxic-ischaemic encephalopathy in asphyxiated newborn infants / S. Futrakul, P. Praisuwanna, P. Thaitumyanon J Med Assoc Thai 2006; 89 (3): 322-8; http://www.medassocthai.org/journal
5. Incidence and prediction of outcome in hypoxic-ischaemic encephalopathy in Japan M. Hayakawa, Y. Ito, S. Saito, N. Mitsuda [et al] Pediatrics International 2014;56:215–221; doi: 10.1111/ped.12233
6. Obstetric aspects of hypoxic ischemic encephalopathy S. Kumar, S. Paterson-Brown Early Hum Dev. 2010 Jun;86(6):339-44. doi: 10.1016/j.earlhumdev.2010.05.009.
7. Perinatal morbidity and risk of hypoxic-ischaemic encephalopathy assotiated with intrapartum sentinel events M. Martinez-Biarge, R. Madero, A. Gonzalez, J. Quero [et al] Am J Obstet Gynecol 2012;206:148-154; doi: 10.1016/j.ajog.2011.09.031
8. Prediction of perinatal hypoxic encephalopathy: proximal risk factors and short-term complications T.Y.Y. Zamzami, S.A. Al-Saedi, A.M. Marzouki, H.A. Nasrat J Clin Gynecol Obstet. 2014;3(3):97-104; doi: http://dx.doi.org/10.14740/jcgo267w
9. Risk factors for low birth weight in Rio Grande do Sul State, Brazil: classical and multilevel analysis A.B. Moraes, R.R. Zanini, J. Riboldi, E.R.J. Giugliani Cad. Saúde Pública, Rio de Janeiro, 28(12):2293-2305, dez, 2012; http://www.scielo.br/pdf/csp/v28n12/08.pdf
10. Risk factors for low birth weight in the public-hospitals at Peshawar, NWFP-Pakistan S. Badshah, L. Mason, K.Mc. Kelvie, R. Payne, P.J.G. Lisboa BMC Public Health 2008, 8:197; doi:10.1186/1471-2458-8-197
11. Risk factors associated with low birth weight of neonates among pregnant women attending a referral hospital in northern Tanzania J.E. Siza Tanzan J Health Res. 2008 Jan;10(1):1-8; http://www.ncbi.nlm.nih.gov/pubmed/18680958
12. Urinary lactate/creatinine ratio as early predictor of hypoxic ischaemic encephalopathy in term neonates admitted to NICU, Zagazing University hospitals M. A. Badr, Y.F. Ali, M. A. Abdelhady [et al.] Res. J. Medicine & Med. Sci. 2011;6(2):54-61; http://www.aensiweb.com/old/rjmms/rjmms/2011/54-61.pdf